RCSEd is committed to the global health priority of patient safety. We aim to do this by providing you, the public, with key information and resources to help you make the best of your surgical journey.
Curated by the College's Patient Safety Group (PSG), these pages will provide a wide variety of resources to support you through every step of your surgical journey, from diagnosis of conditions through to recovery.
You will find generic guides to help you optimise your hospital experience, including specific guides on asking questions, supporting vulnerable groups and consent. We also provide resources to help you prepare for your surgery, providing tips on how to optimise your fitness to help you recover as quickly as possible after your surgery and to reduce the risk of complications.
You will also find links to various subspecialty organisations that will give you more information on your specific condition or type of surgery you are undergoing. This includes information on children’s surgery and dentistry.
The Surgical Journey
You can be referred to the surgical team as an emergency through the emergency on call service or through the outpatient department if your condition does not need immediate attention. It is likely that when you are referred to see a surgeon, your appointment will take place in hospital. Hospitals can be busy, overwhelming places if you have not been before, so do arrive with plenty of time to spare, and do not be frightened to ask a member of staff if you are unsure of where your appointment will be held. Your appointment letter should have details of the department and part of the hospital where your appointment is, including who you will be seeing. If you are anxious about your appointment it may be a good idea to bring someone with you provided this is in line with the hospital’s policy.
During your appointment you will be a seen by a consultant, or a member of their team. There might sometimes be another health professional such as a nurse, dietician or care assistant present depending on the type of clinic. Some appointments may be held virtually but rest assured that the same high standard of care will be provided by your health professional. In these cases, it is important that you have a quiet space with a good internet connection to ensure your appointment goes as smoothly as possible.
During your consultation, your surgeon will ask questions about your health concern, will examine you, and may ask that you undergo some additional tests to give them more information about your condition. They will explain the most likely diagnosis to you, together with risks, benefits and alternatives of any treatment options.
Your surgeon is there to help, so if you have any questions or concerns, please share them with them. After your appointment your surgeon may choose to see you again in a follow up appointment, list you for surgery, refer you to another specialist, or discharge you if they feel you do not need to be seen again. Your surgeon will usually write to your GP or the health professional who referred you to let them know the outcome of your appointment. You can however request a copy of that letter be sent to your home, as some people find this useful for record keeping purposes.
The table below highlights some important things to consider that will help you get the best out of your surgical journey.
- Can we do better
- Patient Prespective
- Empowering the patient
- Ensure mechanisms for feedback and checking patient concerns
- Am I getting equitable care
- How can i ask for it?
- Ensure there is enough time to give this patient the care they need
- Is there enough time?
- How do I ask for more time?
- Consider and account for the patient's ethical/cultural/personal preferences
- Have they considered all my needs?
- How can I highlight them?
- Provide patients with all the information and education they need
- Have they had time to understand
- Have they had the opportunity to ask or enquire
- What additional resources could we provide
- Have I got all the information I need?
- Have I understood it?
- How do I ask for more questions?
- Is there a support group/link/resource I can access on my own?
- Ensure colleagues in primary care have all the information and resources they need if a patient approaches them about their care
- Would my GP be able to give me more information and answer any questions I might have?
- Does my GP have everything I need to know about?
- Ensure patients have the appropriate support structures in place?
- How can we facilitate this?
- Have I got the support I need?
- What do I need to ask for?
- Ensure every patient is given the best care possible?
- What would make it better?
- Am I confident in the care that I have received?
- What more can I want?
- Ensure the healthcare team is accountable for the care delivered?
- Do they know who is responsible for their care?
- Do they know how ti best contact us?
- Do I know what to do if something is not right?
- Do I know who is responsible for my care (came consultant)
- How do I contact them?
- Ensure processes in place to mke any procedure as safe as possible for the patient?
- Do we have the appropriate pre-habilitation/optimisation health structures for our patients before and after their intervention?
- Is there anything I can do to make me healther for my test/procedure?
- Is there anything I should do after my test/procedure?
- Ensure the right feedback loop is in place?
- How do I let my healthcare team know what went well/not so well?

Optimising Your Patient Journey
If you get listed for a surgical procedure, it will either occur as a day-case (going home the same day) or inpatient (going home after at least one night in hospital). You may get a telephone call or further appointment from the Pre-Assessment Clinic Team just before your surgery to ask some detailed questions about your health. This is called a “pre-assessment”, and is conducted by a specialist nurse or an anaesthetist. This is particularly important for people with complex conditions or health needs.
The surgical journey has many stages; this can seem challenging at times. The table below summarizes some ways in which you can optimize your patient journey and help ensure that each stage of your surgical experience goes as smoothly as possible.
Peri-Operative Optimisation: Top Seven Interventions
The Centre for Perioperative Care (CPOC) has developed seven pages dedicated to perioperative optimisation proven to reduce complications by up to 50% for patients.
Click here to read new guidance, infographics and signposting to useful resources on:
- Smoking cessation
- Exercise
- Alcohol moderation
- Practical preparation
- Nutrition
- Mental wellbeing
- Your care, your choice

Making Decisions About Your Care
During your surgical journey, there will be times you have to make decisions with your health professional about what is best for your health. It is vital that these decisions, whether big or small, are made with your thoughts and wishes in mind. Your health professional is there to work with you to ensure that any decision you make together is one that is the safest and best for your situation and takes into account your personal preferences and what is most important to you. As no two patients, even ones with the same condition, are the same, it is important that you have all the information you need to achieve this. You should not feel pressurized to make a particular decision, or feel you have to proceed with a treatment without being comfortable that all questions you have are answered adequately. Ask for more time to consider your options if that would be helpful.
In the medical profession, the patient is at the heart of everything we do. Two gold standard practices in every clinical encounter are shared decision making with patients and facilitating informed consent. Below are some top tips to ensure that you come to the best decisions about your care with your clinician at every stage of your patient journey.
- A good consent discussion takes place in the context of a good conversation between a healthcare professional and patient. It should not be dominated by lots of direct questions from your health professional.
- You should ensure that sufficient time is given to your preferences about your life and your health priorities before making a choice about your treatment.
- Where there is treatment, there is always a choice - even if that alternative choice is no action. Before consenting to a treatment, you should understand what all your options are, even if time is short such as an emergency.
- Major treatment choices should not occur on the basis of a single conversation. If you need time to think about what is best for you, you can ask for a follow up appointment to give you the best chance of making a decision that is right for you.
- Receiving information about your treatment options is not shared decision making with your health professional. Shared decision making involves a discussion about what each option means to you.
- Medical jargon can be very confusing. It is not enough for a doctor or health care professional simply to name the complications associated with a procedure, but they must be able to explain what it means in your particular situation and the chances of it happening to you.
- Your health professional must be completely open and honest regarding the chances of success and failure of each treatment option for your case. This should include the option of doing nothing at all.
- Your health professional may have decision support tools or groups that may help you make the right choice in your care. Feel empowered to ask if aids such as these are available.
- You should be given the option and means to get in touch with your health professional virtually or in person if you have any further questions.
- You should not proceed with any treatment, especially if it is life changing or irreversible, unless you feel this is the right choice for you.

Support for Vulnerable Patients
Our diverse population is made up of people who may need a bit more help that others during their surgical journey. We believe that equity of access for all is am integral part of patient safety. Disability, language or frailty should not be a barrier to accessing the care you need. If you feel that you need more help or support at any point in your journey, you should not be afraid to ask your health professional. The table below outlines some things to consider that may help you get the additional support you need.

Joe Wicks: Get Fit for Surgery – Your Path to Recovery
Joe Wicks helps people get fit for surgery
The CPOC team, the British Geriatrics Society, and Guy's & St Thomas’ NHS Foundation Trust have collaborated with The Body Coach, Joe Wicks, to produce a range of helpful resources aimed at helping people get fit for surgery.
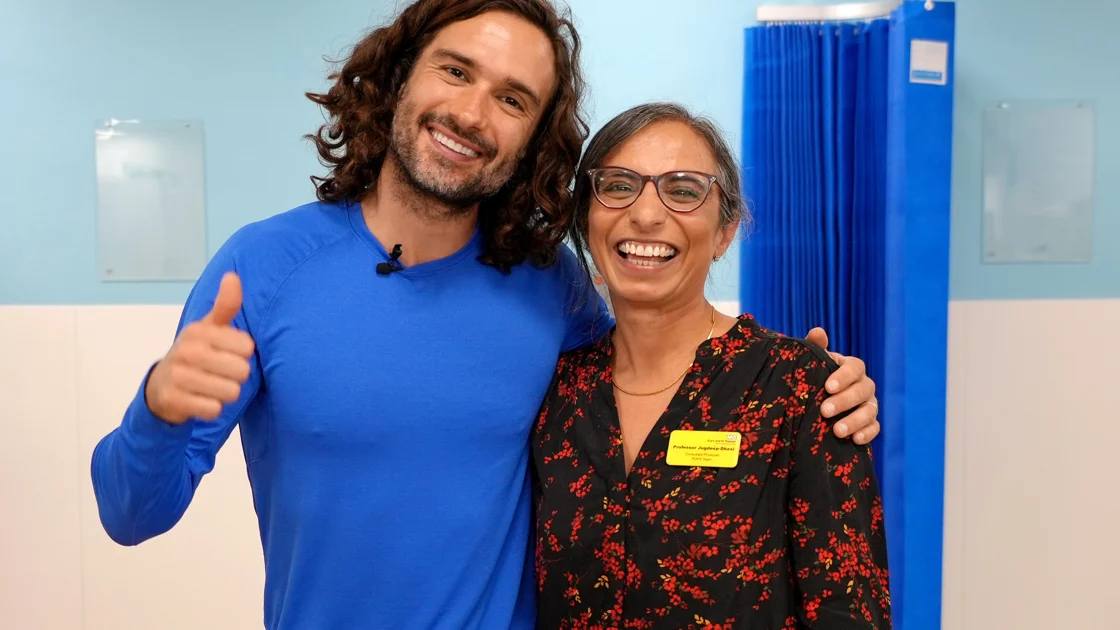
The Centre for Perioperative Care (CPOC) team, the British Geriatric Society (BGS) and Guy's & St Thomas’ NHS Foundation Trust have collaborated with The Body Coach, Joe Wicks, on ways to help people get fit for surgery.
There are 7,000 surgical operations every day in the UK, and up to 1 in 7 people get complications after surgery. This can include issues relating to their wound, heart problems, lung infections and confusion. They can also lose independence if they are in hospital for longer than needed. People who have heart and lung problems, have two or more long-term conditions, and those who are living with frailty are particularly at risk of complications.
Increased activity and improved lifestyle choices ahead of surgery helps reduce these complications. This means patients recover quicker after surgery and get home sooner. It benefits patients, their families and hospitals, which are particularly busy in the winter months.
With the fitness videos, which are on the Bodycoach YouTube channel and CPOC website, Joe Wicks talks to Professor Jugdeep Dhesi, CPOC Deputy Director, about the importance of increasing fitness levels before surgery.
Led by Professor Jugdeep Dhesi, the resources that have been produced are:
• Two 10-min workout videos, with a patient
• Blog from Joe
• Interview with Joe
Resources and Information on Patient Conditions
Below are links to various organisations at can give you more information on specific surgical and dental conditions.

All Surgery and Conditions
Learn More
Childrens' Health
Learn More
Ear, Nose and Throat (ENT)
Learn More
Limbs, Arms and Legs
Learn More
Spine
Learn More
Abdomen
Learn More
Breast
Learn More
Mouth and Teeth
Learn More
Kidneys, Prostate and Bladder
Learn More
Heart and Lung Surgery
Learn More