The modern healthcare system is extremely complex and, with very many integrated parts, it can be difficult to maintain a holistic understanding of patient safety. Following an adverse event, while it is relatively easy to recognize elements retrospectively which were ‘not safe’, recognizing these elements and their relative contribution proactively is much more challenging. Understanding how diverse elements such as training and regulation, local infrastructure, rota design, workplace culture and health care workers wellbeing fit together is essential to be able to proactively manage safety.
The Patient Safety Group have recently undertaken an extensive review of current RCSEd activity to better understand how the College helps to improve patient safety within the wider healthcare system. A ‘human factors’ approach has been used to develop this holistic understanding of safety, providing a global overview of the College’s safety activity and delineating the many elements it can mobilise to support surgical teams in providing safe patient care.
The SEIPS Model
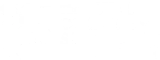
The System Engineering Initiative for Patient Safety (SEIPS) Human Factors model, one of the most popular patient safety systems models worldwide, was used to conduct the inventory. This model, developed in 2006 and funded through the American Agency for Healthcare Research and Quality, helps describe complex modern healthcare systems, recognizing the many interactions and influences between people, tools, tasks, environment, and organizations that contribute to the delivery of safe care.
It breaks the healthcare system into three components: the work system, the care process and the patient outcome. The ‘Work System’ encompasses five interconnected elements: person, tasks, tools and technologies, physical environment and organisational conditions. A person performs a range of tasks using various tools and technologies. The performance of these tasks occurs within a certain physical environment and under specific organisational conditions.
These five interacting elements in turn influence care and other connected processes which in turn impact on patient, staff and organisational outcomes. Staff outcomes include safety, health, satisfaction, stress and burnout; organisational outcomes include rates of turnover, injuries and illnesses, and organisational health. Importantly, it is a dynamic fluid model with any change in one element producing change in the rest of the work system. Staff develop adaptive strategies to perform their tasks, sometimes in response to work systems that are not appropriately designed. Employee and organisational outcomes are addressed along with patient safety, reflecting the fact that patient safety and worker wellbeing are positively correlated and have common system contributing factors.
The model can be used proactively; to design or redesign aspects of a system, or retrospectively examine a system following an adverse event. The model is anchored in the industrial engineering discipline of human factors and endorsed by the UK professional body the Chartered Institute for Ergonomics and Human Factors (CIEHF) which has written is own White Paper on human factors in healthcare, available to view here.
It is clear that Patient Safety is at the forefront of RCSEd endeavour, with a wide range of activity undertaken in all key SEIPS areas. More information on this important work can be seen in our Introductory Video – which gives a brief outline explaining each SEIPS domain - and Interactive Infographic – which provides a short summary of College activity with relevant links in each area.
Learn more about the other areas of the SEIPS model below.
SEIPS Model of Work System and Patient Safety
The PSG at RCSEd has reviewed the College's activities to assess their impact on patient safety within the broader healthcare system. Using the SEIPS Model, the review highlights how interconnected components—people, organisation, technology, tasks, and environment—affect healthcare outcomes. Read more in the 2020 Surgeons' News article below.
Read here

All technology and tools involved in the delivery of healthcare are included in the SEIPS model of patient safety. Technology is spread throughout our whole system; it is used for training, to manage patient flow and monitor elements of population health and, in surgery, often acts as the final interface between provider and patient. Elements may range from IT systems used to manage waiting lists, to new stapling devices for use in laparoscopic surgery.
Technology should be designed to be user-friendly; making it easy to use safely and effectively. As technology evolves we must have pathways to enable safe adoption of the most effective devices. Training must keep pace to ensure providers are adequately trained to use new devices safely.
Activity and Resources
The College continues to invest in newer technology for training; developing webinars, podcasts, blogs, together with other online resources, and courses.
The college has recently joined forces with NHS Highland to establish a new Surgical Education Research and Innovation Lab (SERI Lab), marking a significant leap forward in research of surgical education and innovation.
The College Robotic Surgery Taskforce was formed to consider issues around the implementation of robotic-assisted surgery in the UK and has produced a guidance document that facilitates the development of new robotic services and training in the UK.
The College embraces new technology and develops training courses and programmes to train our members and fellows in emerging techniques, such as Advanced Laparoscopic and Robotic Surgery, for both surgeons and the extended surgical team.
The Definitive Human project, a virtual reality anatomical resource, is being developed in conjunction with Glasgow College of Art.
Collaboration with industry partners Younger Fellows' Group allows the College to ensure training in newer technologies is available to Members & Fellows.
The College has embraced the use of simulation in training; recently accrediting the Dundee Institute for Healthcare Simulation.Younger Fellows Group
The Younger Fellows' Group holds workshops on ergonomics and the use of energy devices within theatre.
As technology and new tools become available, it is the responsibility of all healthcare professionals to make use of these where possible to enhance practices and continue to drive increased standards.
Top 10 Tips for Surgical Safety
Claire Morgan, PSG member, outlines the top 10 tips for surgical safety using the Safety Engineering Initiative for Patient Safety (SEIPS) framework. The document highlights key principles such as putting patients at the centre of care, ensuring team well-being, working within skill sets, using surgical safety checklists, fostering a just culture, learning from mistakes and considering human factors and ergonomics in the surgical environment. Each tip is supported by evidence and links to further resources.
Top 10 Tips for Surgical Safety
Click on the link below to read the top 10 tips for surgical safety document.
Read hereInformation for Patients - Patient Safety
Surgery is often required to treat disease and save lives, but there is always the potential for surgical treatment to cause harm. Keeping patients safe during their treatment is a fundamental part of surgical practice, and patient safety is embedded within the core values of the College.
With this in mind, the Patient Safety Group at the Royal College of Surgeons of Edinburgh has undertaken an extensive review of all college activity, with the aim of identifying areas of our work that influence patient safety within the wider healthcare system.
Surgical care is complex and recognising all the factors that contribute to good patient outcomes can be difficult. Many industries have taken a Human Factors approach in order to better understand this complexity. Human factors is a scientific discipline that aims to study human, technology, and systems interactions, in complex environments, such as healthcare.
A Human Factors approach has been applied here, using the Systems Engineering Initiative for Patient Safety or SEIPS Model. The SEIPS Model breaks down surgical care into 5 component parts; Person, Organisation, Environment, Technology and Tools, and Tasks, recognising that all of these parts interact. These five component parts each influence care processes which in turn influence care outcomes.
The webpages included in the patient safety inventory are available for patients and will be used by our members as a resource for patient safety education. They cover the College’s patient safety activities and contain information, tools, and additional resources, presented using the SEIPS Model.
By adopting this systematic approach to safety, the College has an objective way of understanding, reviewing, and improving patient safety. It can ensure that all of its activity is aligned enabling it to better meet its strategic goal of ensuring the best possible outcomes for patients worldwide.
Resources and Information for Patients, Families and Carers
The Patient Safety Group have developed a range of resources to help support patients, together with their families and carers, during their surgical journey, from initial referral, through outpatient or emergency consultation, to preparation for and recovery from surgery.
Learn more