The Patient Safety Group (PSG) of the Royal College of Surgeons of Edinburgh (RCSEd) are delighted to lend our enthusiastic support to the sixth World Patient Safety Day (WPSD). This event, established by the World Health Organisation (WHO) in 2019, takes place on 17 September every year. It helps to raise global awareness amongst all stakeholders about key Patient Safety issues and foster collaboration between patients, health care workers, health care leaders and policy makers to improve patient safety. Each year a new theme is selected to highlight a priority patient safety area for action.
The theme set by the WHO for this year’s WPSD is “Improving diagnosis for patient safety”, recognising the vital importance of correct and timely diagnosis in ensuring patient safety and improving health outcomes.
I. DIAGNOSTIC SAFETY AND DENTISTRY WPSD 2024
With the theme of WHO World Patient Safety Day: Improving Diagnosis for Safety, this should be considered in all healthcare settings with Oral Health as no exception. Diagnostic error is the cause of 16% of preventable harms recorded globally (WHO, 2024). As in all health care, dental diagnosis is complex involving gathering, integrating, and interpreting information which at any stage can result in a missed, delayed, or incorrect diagnosis. Globally, oral disease is the most prevalent of all noncommunicable diseases (NCDs) with the most common conditions: decay (caries) and gum disease (severe periodontitis) (WHO, 2022). With correct diagnoses delivered in a timely manner, dentists can offer their patients appropriate individualised treatment options, supporting shared decision making for treatment and ongoing referral if required. However, with multiple sources of information clinical decision making is often simplified in diagnosis and treatment of oral/dental disease, with reliance on intuition and heuristics which can lead to patient harm (Murdoch et al, 2023).

II. STEPS TO DIAGNOSIS
1. Patient presentation
Patient education is essential to ensure they know the benefits of seeking help when symptoms arise. This is particularly important in oral cancer and highlighted by several healthcare campaigns (Barrett et al, 2023). Equally healthcare practitioners should be appropriately aware of oral cancer occurring in any patient whatever their age, as so eloquently described by Barbara Foutain founder of the charity Young Tongues in our September issue of Surgeons News.
Equally we need to educate our patients to ensure regular oral health review, so that prevention and treatment can be instigated early; the most common oral diseases caries and periodontal disease are largely preventable. Patient presentation is often forgotten in the diagnostic journey, though obviously can be affected by access to primary dental care, which is currently an issue in the NHS as challenged by the RCSEd. (https://www.rcsed.ac.uk/media/1333989/rcsed-fds-dental-manifesto-2024.pdf).
2. Patient history and examination
It is acknowledged that history taking may be one of the most important stages in a patient’s pathway to diagnosis and treatment. In dentistry the history should include taking medical history for direct patient safety reasons, but also dental history and symptom/pain history. A thorough oral examination including: extraoral TMJ, asymmetry, nodes and, facial skin; and intraoral mucosa, periodontal, hard tissues, occlusion and, tooth wear, will then allow for prescription of appropriate diagnostic tests where needed.
All hospital inpatients require an oral assessment with appropriate oral health care plan; the mouth can provide signs to help overall diagnosis particularly in the elderly and those who cannot communicate (Doshi & Patel, 2017). Dr Doshi subsequently launched the Mouth Care Matters Campaign was developed as a training initiative for healthcare workers to improve the oral health of hospitalised patients. (https://mouthcarematters.hee.nhs.uk/wp-content/uploads/sites/6/2020/01/MCM-GUIDE-2019-Final.pdf)
3. Diagnostic testing and interpretation
Dentists assign diagnostic tests to ‘special tests’ which include: nerve testing (sensibility), imaging (radiographs and cone beam CTs), diagnostic models (study casts), sampling (mucosal biopsy, pus aspiration/swab). Radiographic reporting is done by dentists and, CBCT reporting where qualified to do so (Brown et al, 2014). Time to assess and report on radiographs by dentists is thought to be a major contributing factor to diagnostic error (Hedge 2023, Plessas et al, 2019).
The biggest change in dentistry in recent years has been evolution of the digital workflow which impacts on every step of patients’ pathways including diagnosis. Although AI is considered a huge potential advance, the rapid development of new technologies themselves, also potentially present a safety challenge (Gross et al, 2019).
4. Communicating results
Communication of results not only to patients but other healthcare workers is another risk to patient safety and diagnosis. There must be clear pathways for this to happen, particularly when onward referral is required as transitions in care are a big risk to patient safety. When communicating with patients we must ensure we present this information tailored to their needs (https://www.england.nhs.uk/publication/accessible-information-standard-specification/). Patients themselves believe lack of self advocacy and poor health literacy are some of the main contributors to diagnostic error (Obadan-Udah etal, 2024).
Diagnosis, treatment and evaluation
Dental Pain
Identifying the cause of patients’ dental/referred pain in the oral cavity is an essential skill for all dentists (Renton, 2011), though can be challenged when encountering distressed and sometimes anxious patients. Causes of dental pain or referred dental pain can include: reversible pulpitis, acute pulpitis, apical periodontitis, perio-endo lesion, periodontal abscess, atypical facial pain, mandibular dysfunction which all warrant completely different treatment. Cracked tooth syndrome presents its own diagnostic dilemma with, unfavourable sequalae including catastrophic tooth fracture if not diagnosed and left untreated (Hasan et al, 2015)
Oral Infection
Oral infection too must be addressed by dentists and treated appropriately. Dental infection can lead to airway obstruction and sepsis (https://www.england.nhs.uk/ourwork/clinical-policy/sepsis/sepsis-frequently-asked-questions/); as reported during the COVID pandemic a delay in diagnosis can result in serious complications particularly in those who are medically compromised (Altrias et al, 2022). Antibiotic prescription must be appropriate as described by Noha Seoudi, Oral Microbiologist in our September issue of Surgeons News; and following current guidance (https://cgdent.uk/antimicrobial-prescribing-in-dentistry/). Pulpitis is not an infective condition and should not be managed with antibiotics; similarly localised infection should not be managed with carte balance antibiotic prescription.
Trauma, Tooth Wear and Periodontal Disease
Tooth ache or nerve pain symptoms should be diagnosed and managed by applying basic endodontic principles to ensure appropriate treatment (https://britishendodonticsociety.org.uk/_userfiles/pages/files/a4_bes_guidelines_2022_hyperlinked_final.pdf). Equally, endodontic damage from trauma requires correct diagnosis again to inform appropriate management. (https://www.dentaltrauma.co.uk/Guidelines.aspx).
Other examples in dentistry where diagnosis is essential is tooth wear caused by grinding (attrition), acid (erosion) and rubbing (abrasion). Each different cause of tooth wear requires different management (https://www.bsrd.org.uk/File.ashx?id=15192).
In gum disease, (periodontal) all too often late diagnosis, escalates problems for patients. Screening for periodontal disease is an essential part of all dental consultations to ensure patients are managed in a timely fashion. In 2017 a new classification of periodontal disease was adopted based on 4 stages of severity and, 3 grades of progression; one study showed a 30% diagnostic error using the new classification (Tokede et al, 2024). Management is all important in periodontal disease with early diagnosis, prevention and referral to specialist services where appropriate. The impacts of periodontal disease on general health should considered in terms of diabetes, and potentially cardiac and pre-term babies along with other medical conditions (https://www.bsperio.org.uk/).
Oral Medicine, Oral Surgery and Orthodontics
This blog is very focussed on Restorative Dentistry, though diagnostic dilemmas exist in other dental clinical specialties. For example, Oral Medicine which focuses on oral mucosal disease which may have serious implications and be a sign of systemic disease such as: pemphigus vulgaris, lupus, HIV, acute myeloid leukaemia or Vitamin deficiencies. Oral medicine also manage and diagnose dysplasia and oral cancer. Oral surgery diagnosis presents similar dilemma in terms of diagnosis, and the reason for extraction ie diagnosis must be discussed with the patient both at diagnosis and consent. Orthodontic diagnosis is essential to ensure a good outcome from treatment (Uribe et al, 2015)
III. DIAGNOSIS AND A SYSTEMS ENGINEERING INITIATIVE FOR PATIENT SAFETY (SEIPS)
The linear approach described in the dental diagnostic process outlines the steps and process. However, diagnosis is not a linear process and when diagnostic error occurs, all the interacting systems at play in the complex socio-technical system of healthcare should be considered. A work systems factors approach facilitates consideration of the role of these contributory factors involved in the patient safety diagnostic pathway; the systems include person, internal organisation, environment, tasks, tools, technology and external environment.
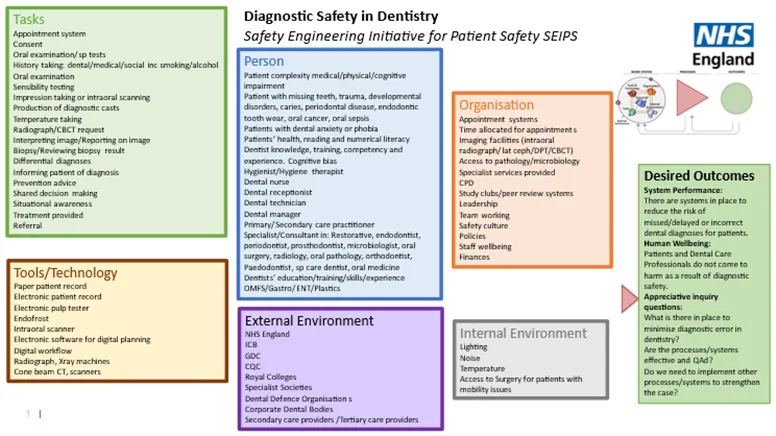
Think of a scenario where through Root Cause Analysis an individual was thought to be the cause of misdiagnosis in dentistry, if improvement is focused on the individual then what is to stop another individual making the same diagnostic error? SEIPS as first described by Carayon in 2006, is a work systems factors approach that can be used to analyse patient safety incidents including dentistry. NHS England have recommended the SEIPS tool to understand patient safety incidents under the patient safety incident response framework (PSIRF - https://www.england.nhs.uk/patient-safety/patient-safety-insight/incident-response-framework/). SEIPS can be applied as general ‘problem-solving tool e.g. to guide how we learn and improve following a patient safety incident, to conduct a horizon scan, and to inform work system factors design.’ (https://www.england.nhs.uk/wp-content/uploads/2022/08/B1465-SEIPS-quick-reference-and-work-system-explorer-v1-FINAL.pdf).
Strategies to improve diagnostic safety in dentistry can be developed from SEIPS and feed into improvement pathways. The literature suggests diagnostic safety in dentistry can be improved by: taking adequate time when investigating a case, forming study groups, increasing communication and, putting more emphasis on differential diagnosis (Nicdel et al, 2018).
Key Messages for Diagnostic Safety in Dentistry
Written by Claire Morgan, Deputy Chair for Patient Safety Group and Dental Council RCSEd, Consultant in Restorative Dentistry, Patient Safety Specialist Bart Health Trust