A collaborative approach between the regional Maxillofacial Unit, QEUH. Glasgow and the Emergency Medicine teams, Glasgow.
In the management of any surgical emergency, patient safety is of critical importance. The key step is the recognition of the condition and the next is alerting the appropriate set of clinicians with the experience and skill set to manage the emergency in a timely manner. Head and neck necrotising fasciitis is such an emergency with timely surgical debridement the only intervention with good evidence to suggest improved outcomes. Diagnosis of necrotising soft tissue infections has been described as a significant challenge. This can lead to delays in treatment. Diagnosis relies on evaluation of clinical signs, interpretation of radiological investigations and biochemical parameters. The “Laboratory risk indicator for necrotising fasciitis score” (LRINEC) has been utilised as an adjunct to aid in diagnosis with an applicable degree of sensitivity.
In recent years, particularly 2022-2023, our unit has seen unprecedented numbers of patients presenting with head and neck necrotising fasciitis potentially related to increased Group A Streptococcus circulating in the Scottish population post-COVID pandemic. We encountered a number of cases with treatment being delayed either due to the fact that the condition was not recognised on admission or the patient was referred to another speciality that did not manage the patient as a surgical emergency.
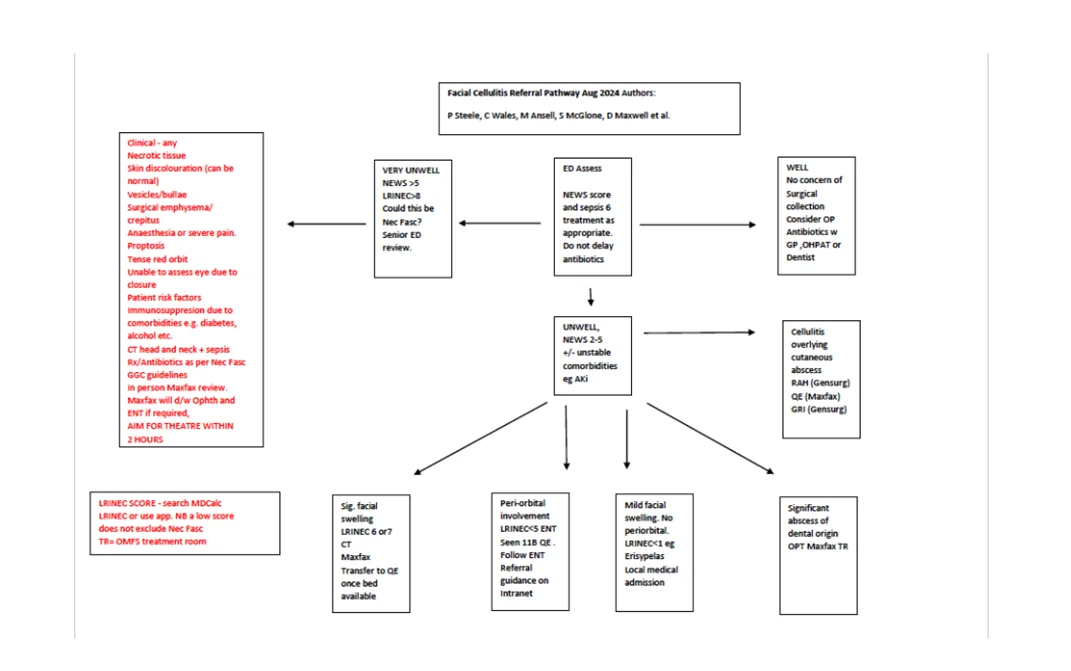
We attributed some of these errors to a complicated referral pathway for Emergency Medicine departments. Particularly in the paediatric setting, peri-orbital cellulitis has been managed by Ophthalmologists and ENT as the specialities best equipped to manage the condition when related to sinus disease or an orbital sub periosteal abscess. The referral pathway for facial cellulitis has been a source of frustration for our colleagues in Emergency Medicine. Surgical specialities can be reluctant to admit patients with facial cellulitis without overt indications for surgical intervention and we have found in many instances physicians have reported being unfamiliar managing the condition. Both elements lead to delayed recognition and definitive treatment.
We evaluated 39 patients presenting with head and neck necrotising fasciitis. Some of our key findings were that patients admitted from Emergency Medicine with a speciality other than OMFS waited longer for surgical management compared to those directly referred directly to OMFS. We also found that many cases demonstrated similar biochemical parameters on admission, with only 4 patients having an LRINEC score less than 6.
We have produced a local pathway to help identify patients presenting with head and neck necrotising fasciitis earlier and enable our Emergency Medicine departments provide a clear referral pathway for facial and peri-orbital cellulitis.
Written by Mr Peter Steele. Consultant OMFS/ Head & neck Surgeon, Regional Maxillofacial Unit. QEUH, Glasgow